- Life expectancy at birth in developed countries is longer than at any time in history and more than double what it was for millennia before the 1800s.
- Across wealthy countries it has been increasing at a rate of roughly 2.5 years per decade for more than a century and a half, a process in which Germany, France, Austria and Switzerland have clearly participated.
- Until several decades ago, the extension of average life expectancy came from preventing early death. Since the 1970s, though, it has overwhelmingly come from reduced mortality among those over 65, as more people than ever live into their 80s, 90s and 100s.
- These later life years, while not free of chronic disease, are ones in which most people can live autonomously.
- Societies are now faced with the opportunity and challenge of how to help individuals reap the benefits of this additional time.
“Current levels of longevity are totally unprecedented,” says Professor James Vaupel, founding director of the Max Planck Institute for Demographic Research in Rostock, Germany. “Humans have never lived anything near as long as now.”
Today’s extensive life spans are the most surprising chapter in a story of increasing human longevity that began during the better part of two centuries ago. One way to understand this process is to look at the average life spans of women—consistently the longer-lived gender—in the country with the greatest life expectancy.
History’s arc
Worldwide, archaeological evidence and diverse historical documents all indicate that for millennia human life expectancy remained consistently between 25-35 years of age. By the 1840s, in some parts of Europe, this figure had climbed slightly, to about 45 years. Since that time, however, with what Professor Vaupel calls “amazingly consistency”, best-practice female life expectancy has risen by around 2.5 years per decade, so that now the average woman in Japan will reach the age of 87. The same trend occurred slightly later in male life expectancy.
The phenomenon in individual countries, such as Switzerland, France, Germany and Austria, is not so simple: different starting points for the process, major wars, epidemics and even occasional pauses have all prevented such sharp linearity. Nevertheless, the underlying trend in each of these four countries has been a clear upward trajectory.
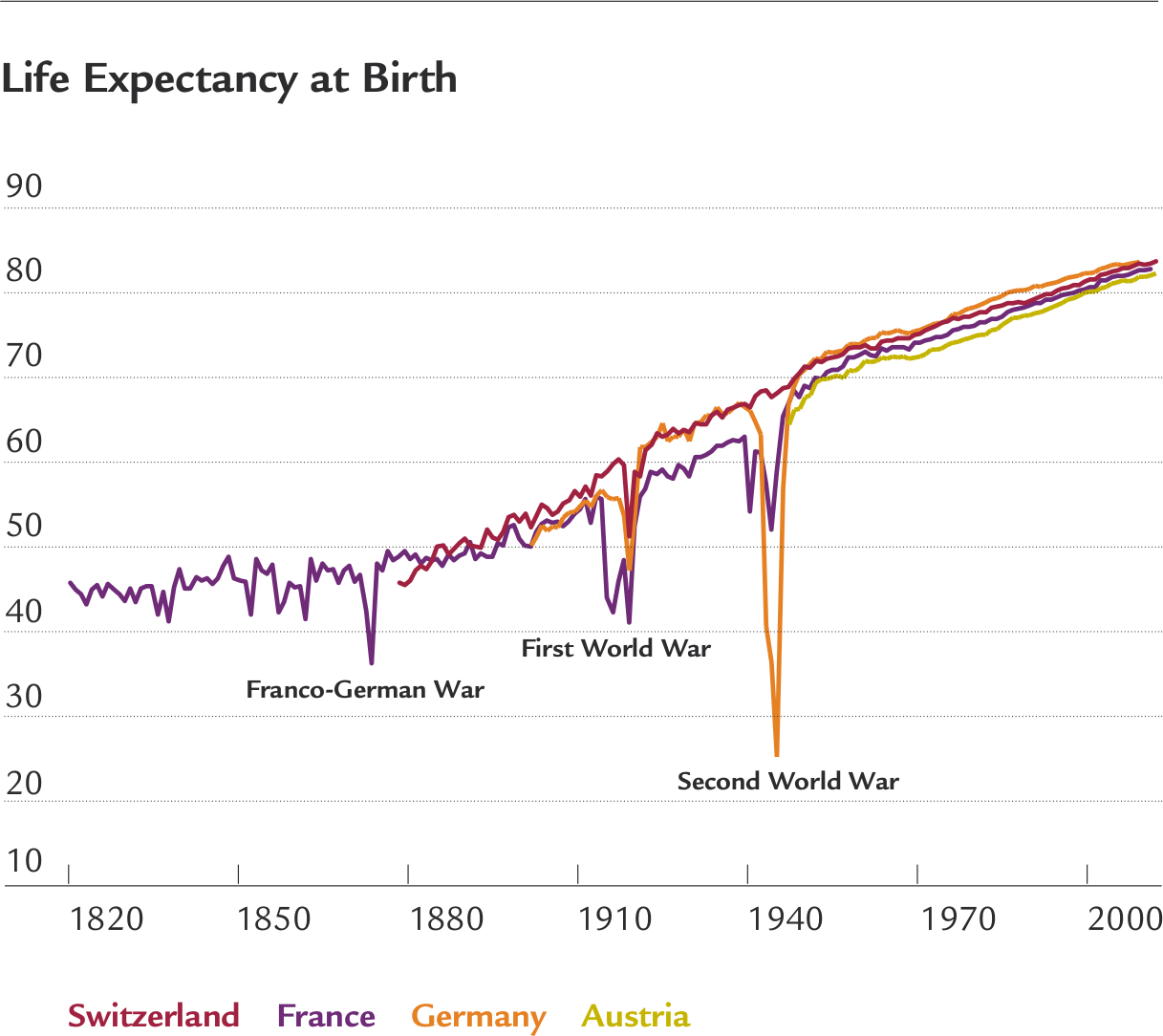
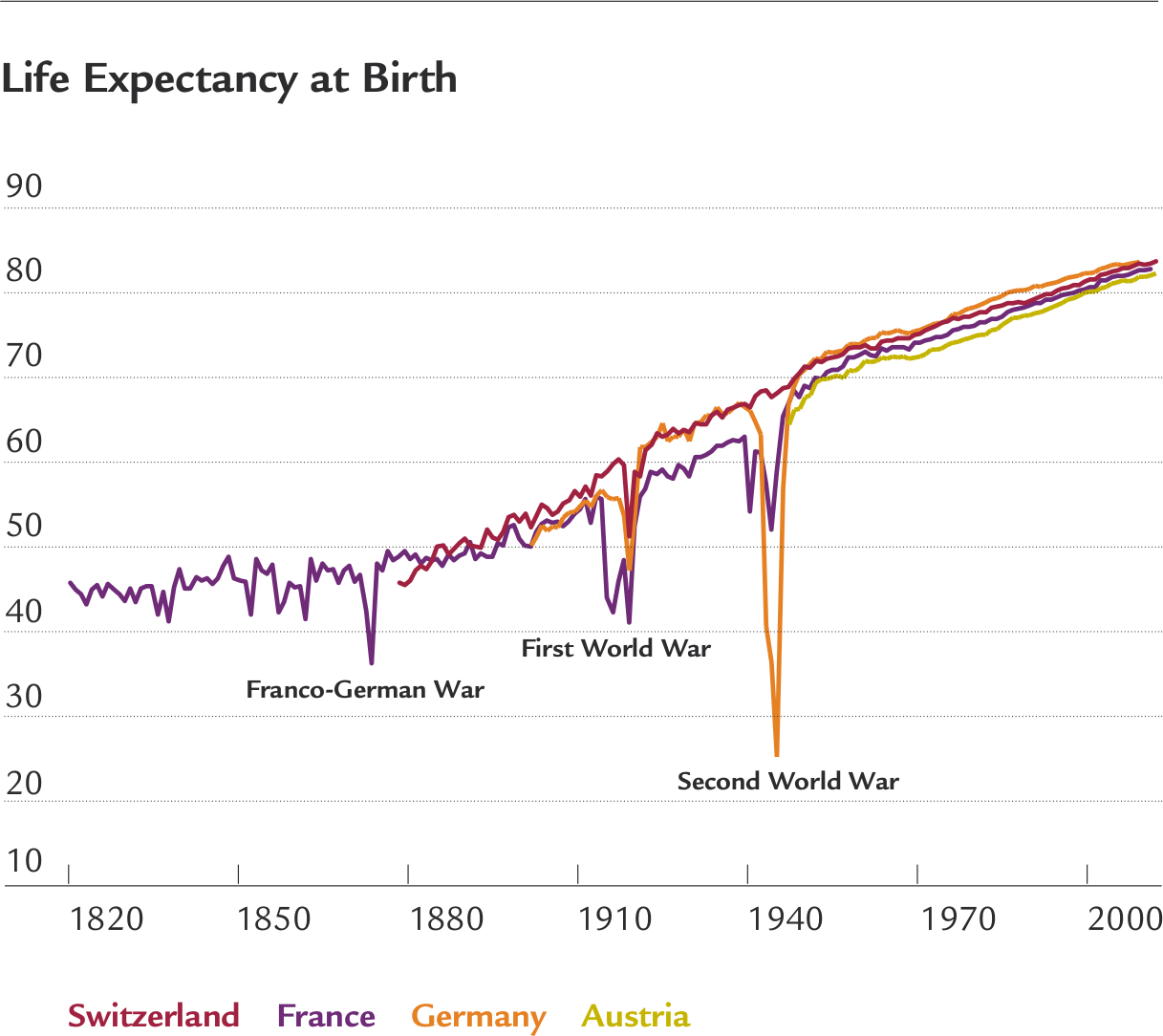
While the speed at which life expectancy has grown has been consistent, the drivers of this change have varied over time. The resulting series of partially overlapping developments has largely occurred in the same order across every developed country.
Leaving behind infant mortality
Historically, until well into the 20th century, the first year of life was by far the most dangerous in terms of mortality. Indeed, in France it was not until the 1920s that the number of those dying before they reached one year dropped below 10% of the total in any given year—a figure which already represented a huge improvement over preceding decades. During the late 19th and throughout much of the 20th century better public health, improved nutrition and more effective medical care combined to eliminate the vast majority of infant deaths in developed countries.
Progress in infant health continues: in Switzerland, France, Germany and Austria well below one child out of 250 dies before its first birthday. By the mid-1900s improvements in early childhood mortality across the developed world had been so successful that they offered little room to improve life expectancy further.
Average life spans continued to rise, but the majority of the gains were then among working-age adults. These were for the most part people aged between 40 and 65. The process began before the second world war and thereafter became the dominant contribution to life expectancy gains as those from infant mortality tailed off. The chart below of French survival curves shows the number of people surviving from a notional cohort of 100,000 people born at different points in time. As the lines stretch out first there are gains through the reduction of childhood mortality and then improvements in middle age before extension to later life.


Nothing new under the sun
Although clearly very positive, until the 1980s in most developed countries these gains in life expectancy did not present societies with anything they had not seen before. Instead of dying young, more people were living to an older age, which a noticeable, if small, proportion of the population had always reached. The outer limits of age did not seem to be shifting greatly; the number of those living to 100 or beyond had not increased.
The conventional wisdom among demographers and biologists was that a notional upper time limit existed beyond which human bodies were unable to live. Average life expectancy was expected to cease its upward march as medicine allowed more and more people, having lived mostly healthy lives, to approach or reach that limit. Thereafter, the vast majority would pass on relatively quickly owing to the boundaries of biology. “This is basically what everybody was thinking until about the year 2000,” notes Jean-Marie Robine, a research director at the French National Institute of Health and Medical Research in Paris.
The longevity revolution
Hundreds of years of academic consensus were overturned as developed countries underwent what demographers call the “longevity revolution”. Although not obvious to demographers at first, “since about the 1970s gains in life expectancy have come from reducing mortality among those ofer 65,” says Professor Vaupel. This, he adds, occurred both because people were reaching that age in a healthier state than their ancestors and as a result of public-health and medical progress in the fight against certain diseases likely to affect this group, such as cardiovascular disease and cancer.
The latest phase in this rise in longevity has brought with it two entirely unexpected statistical shifts. First, the age at which death is most common—the so-called modal age at death—has moved steadily higher. Switzerland is representative here: discounting infant mortality, the modal age of death rose from 75 in 1926 to 80 in 1970, which was consistent with expectations of more people reaching a notional human age limit. Since 1970, however, life expectancy has risen to 89 at a steady pace of more than two years per decade. At the same time, the upper age limit to which no more than a handful can aspire has also risen steadily. In a number of European countries, including Switzerland, France, Germany and Austria, “the number of centenarians has been doubling every decade for around 50 years”, notes Professor Robine. In parallel, Professor Vaupel expects that most people born today in developed countries will live to the age of 100.

The rise of a fourth age
Recent developments in longevity have reversed long-standing statistical assumptions, according to Professor Robine. But, he adds, they are truly revolutionary because they are “effectively breaking all our conceptual frameworks”. The life course, for example, has traditionally been divided into three parts—childhood and youth, or those aged up to about 20 years; working adults up to 65; and old-age thereafter. This framework seemed sound through decades of increasing life spans because most people were still dying in their 70s. “Today,” Professor Robine says, “it is no longer working. We now may have four generations in same family and a ‘fourth age’ in society: the young, the adult working, seniors, and the oldest old.” This is in effect a new stage in life which previous generations rarely experienced.
But are these extra years healthy or do they simply represent unwelcome decades of illness at the end of life? This may pose a false dichotomy. If health is defined merely as the absence of disease, then these years are unhealthy indeed. Figures vary, but EU statistics usually estimate that 80% of those over 65 have at least one chronic condition.
Not simply sick or well
Absence of disease, however, which worked as a definition of health in an earlier era, is a problematic one in societies where many chronic conditions can be well controlled and have little or no effect on personal autonomy. Professor Robine notes that “today people are more robust and less frail. Old-age-related mortality is occurring later.” In such a situation, he adds, “we have to define what being healthy is when you are 85 years old or among the oldest old and when you have several co-morbidities but still have potentially many basic capacities.”
Professor Vaupel explains that a better gauge of overall health “is to ask if people can take care of themselves—live alone, get dressed, wash, eat food—and if they can think clearly”. By this measure, healthy life years are increasing at about the same rate as overall life expectancy. He notes that “75 is the new 65, with today’s 75-year-olds as healthy as 65-year-olds were five decades ago”.
The extent to which healthy life years are increasing at older age levels is less clear, simply because the relevant age groups have been too small to study until very recently. Going to the current edge of extreme old age, though, it is harder to be certain about changes to health. Professor Robine notes that a study of centenarians in Denmark suggests that later cohorts are healthier than earlier ones, although data from Japan suggest the opposite.
Breaking through upper limits
Whatever the situation at the frontier of human longevity, it seems clear that the growth in life expectancy has increased—and will continue to increase—the average number of years in which humans can continue to live active, independent and autonomous lives.
Given the fact that we are now living with an unprecedented number of citizens over 65, it is reasonable to wonder how long life expectancies will keep growing. Professor Vaupel and Professor Robine each warn that this is impossible to predict accurately, but both expect current trends to continue for some time. Professor Vaupel sees “no compelling evidence that we are approaching a looming limit in life span and no biological reason why there should be”. He acknowledges that, given already low mortality rates elsewhere, this will require improvements to the health of those currently in their 70s, 80s and 90s, but new research and technologies may well provide these.
Redefining longer lives
Professor Robine adds that, even without any medical breakthroughs, further steady gains are likely. Since factors such as maternal and early childhood conditions have such an impact on life expectancy, current increases owe something to public-health and nutrition improvements that occurred decades ago. But how are individuals and society going to take advantage of these extra years? Many individuals will enjoy unprecedented leisure opportunities, the chance to connect more deeply with their families, or the possibility to shift gears professionally.
Signs of change already exist. According to OECD data, between 2000 and 2014 the labour force participation rate among those aged 65-69 has risen. But the wide variation in these rates between countries—for those aged over 65 it is 5.9% in France, 14% in Germany and 22.4% in Switzerland—indicates that cultural expectations and government policies will have a profound effect on the choices open to this growing population of older citizens.
Too often the very novelty of conditions created by the longevity revolution has left us culturally and politically unprepared. Professor Vaupel believes that “most people are not mentally ready. When they think about old age, they think about their grandparents and parents. They don’t realise they will be healthier.” Professor Robine adds that, looking beyond the individual, “society is still organised assuming the division of the population into only the young, working adults and seniors. Policymakers still think in these frameworks.” Going beyond simply re-evaluating such past conceptions, individuals and societies must embrace the chance to derive greater value and meaning from this new fourth stage of life.
Written by




![Little Old Lady with her Pets enjoying Summer on the Balcony.
Please see more similar images here:[url=http://www.istockphoto.com/file_search.php?action=file&lightboxID=8234435]
[img]http://s700.photobucket.com/albums/ww8/bi_bi/lightboxes/lifestyle.jpg[/img][/url]](/content/internet/com/en/home/blog/stadtentwicklung-demografischer-wandel/_jcr_content/moodimagearticle/image.1558701378981.transform/16_9_3840w/Seniors_are_going_to_town.jpg)
